
It has become evident by changes to the Centers for Medicare & Medicaid Services (CMS) Star Rating formulas over the past several years—and especially with changes implemented for the 2021 Plan Year—that member experience and medication adherence is of utmost importance to the CMS. Medicare Star Ratings measures are primarily calculated based on Healthcare Effectiveness Data and Information Set (HEDIS) as well as Consumer Assessment of Healthcare Providers and Systems (CAHPS) data.
HEDIS consists of a standardized set of performance measures used to rate health plan performance with respect to health issues, including cancer, smoking, heart disease, diabetes and asthma.
CAHPS data is developed using a set of surveys that primarily measure the patient or member experience as they interact with health plans and health care providers, including doctors, nurses, and others in various settings, including hospitals, physician offices, and other healthcare facilities.
The Star Rating assigned to each Medicare Advantage (Part C) and Part D (Prescription Drug) Plan is calculated using the weighted average of various quality measures. This is a bit of an oversimplification of the process as there are 34 measurements for Part C plans and 14 measurements for Part D plans, and the calculations and data sets are quite complex.
As we mentioned earlier, there are quite a few changes in how the 2021 Medicare Star Ratings get calculated. These changes give significantly more weight to the member experience measures. The following section provides a synopsis of the changes for 2021.
Medicare Star Ratings 2021 Changes
The CMS has increased the weight of patient experience measures, which are determined by CAHPS as well as member complaints, health care access, members choosing to leave the plan, appeals, and call center measures, all of which reflect overall member experience. The weight of these measures moved up from 1.5 to 2 for the 2021 Plan-year Star Ratings. Additionally, the CMS finalized its proposal to increase the weight of these member experience measures from 2 to 4, starting with the 2023 Plan Year Star Ratings.
Important Medicare Star Rating changes from plan-year 2020 to 2021
| 2020 | 2021 | |
|---|---|---|
| Changed | Part C and Part D improvement measures (C30 & D06) for MA-PD contracts Part D measure Drug Safety and Accuracy of Drug Pricing: D10, D11, D12, D13, &D14Comprised of 2018 HEDIS & 2019 CAHPS data | Member Experience and Access categories changing from 1.5x to 2.0x Statin Use in People with Diabetes Measure increased to 3Revised Plan Makes Timely Decisions about Appeals2022 Star Ratings will be comprised of 2020 HEDIS, 2020 HOS, and 2021 CAHPS data |
| Transition of a Measure | Part C measure – Controlling Blood Pressure was temporarily moved to the display page for the 2020 and 2021 Star Ratings because NCQA made substantive changes to the measure specification | Part C measure – Plan All-Cause Readmissions was temporarily moved to the display page for the 2021 and 2022 Star Ratings because NCQA made substantive changes to the measure specification |
| Retired Measures | Changes to the Plan All-Cause Readmissions measure will retire it from the 2021 and 2022 ratings | None |
Medicare Star Ratings 2021 Performance Overview
As a result of changes to the CMS star ratings 2021 calculations, and the impact of the Covid-19 pandemic, the 2021 Star Ratings were calculated differently than usual. 2021 Star Rating values based on HEDIS and CAHPS were replaced with values from 2020 Star Ratings (care delivered in 2018). However, there was still an impact on overall Medicare Star Ratings from the previous year.
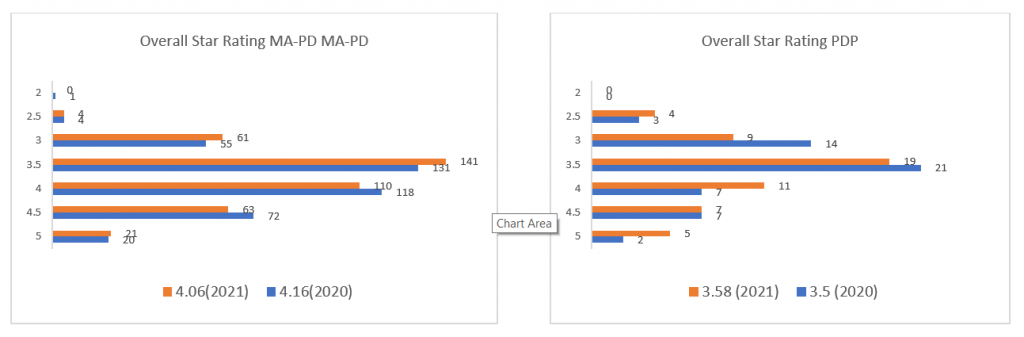
Of the 400 rated plans, 72 plans were rated at 4.5 Stars in 2020; that number dropped to 63 plans in 2021. The number of 5-star rated plans increased by 1 from 20 to 21 in 2021. The graphs below show the movement across all Star Ratings for Medicare Advantage and Part D plans from 2020 to 2021.
These changes in the Star Rating measures and weights emphasize the CMS’ continued focus on member experience, but in a way that has more significant financial impact through the Quality Bonus Payments (QBP), which is based on Star Ratings. Those plans that execute well with respect to member experience will be rewarded with higher Medicare Star Ratings and a higher QBP, which translates into a increased rebate share. This allows those plans to maintain or increase the benefits provided to their members and mitigate increases in member premiums, all of which will position the plan for greater member growth and profitability.
How To Improve CMS Star Ratings
Member Experience, Complaints and Access Measures
The need for solutions to maximize member-experience measures will be greater than ever as we move forward, and the weight of those measures continues to increase. Star measures are continually shifting as the bar continues to be raised. Inovaare solutions help ensure those at health plans with responsibility for overall Medicare Star Ratings, as well as those teams with responsibility for individual measures, have the tools and systems in place to ensure Star Ratings are maximized. Medicare Stars expertise—combined with the systems and tools in place to support internal Stars teams—are essential for health plan growth and financial success, especially concerning the member experience measures listed below, which are more important than ever.
| Part C Measures | Part D Measures |
|---|---|
| Getting Needed Care (CAHPS) | Call Center – Foreign Language Interpreter and TTY Availability |
| Getting Appointments and Care Quickly (CAHPS) | Appeals Auto-Forward* |
| Customer Service (CAHPS) | Appeals Upheld* |
| Rating of Health Care Quality (CAHPS) | Rating of Drug Plan (CAHPS) |
| Rating of Health Plan (CAHPS) | Getting Needed Prescription Drugs (CAHPS) |
| Care Coordination (CAHPS) | Drug Plan Complaints* |
| Complaints about the Health Plan* | |
| Members Choosing to Leave the Plan | |
| Plan Makes Timely Decisions about Appeals* | |
| Reviewing Appeals Decisions* | |
| Call Center – Foreign Language Interpreter and TTY Availability |
*Inovaare solutions are available to assist with improving this member experience measure.
Looking Ahead
Inovaare can help Medicare Advantage plans and providers deliver quality care and improve customer experience measures to increase Medicare Star Ratings, with a goal of achieving a 5-star rating, by implementing either our new A&G Pro 30 or A&G Enterprise solution. A&G Pro 30 is an out-of-the-box solution that can be implemented within 30 days to lower operating costs and improve the member experience. It also provides health plans with end-to-end visibility of real-time data for accurate monitoring, better decision making and expedited resolutions.
For health plans that require high levels of customization, Inovaare’s A&G Enterprise solution can be implemented. Supported by A&G professionals with decades of leadership experience in health plan appeals and grievances departments, A&G Enterprise ensures payers receive a tailored system that best suits their unique needs along with industry consultants who can help ensure best practices are built into the customized solution.
Inovaare provides highly configurable healthcare payer-specific software solutions that automate quality and compliance operations. We help organizations reduce risk, increase compliance visibility, lower operational costs and improve their oversight process.
FOR MORE INFORMATION, visit www.inovaare.com or call 408-850-2235
For additional information on the changes and updates to the 2021 Star Ratings system, https://www.cms.gov/files/document/2021starratingsfactsheet-10-13-2020.pdf
Overall Star Rating Distribution for MA-PD Contract https://www.cms.gov/files/document/2021starratingsfactsheet-10-13-2020.pdf
Weight of Patients’ Experience and Complaints Measures and Access Measures pg: 33892 https://www.govinfo.gov/content/pkg/FR-2020-06-02/pdf/2020-11342.pdf
Craig Giangregorio, A&G Industry Expert

