Healthcare Cloud Platform
Seamless Data Management, Compliance, Operations, and Member Service
Error: Contact form not found.
Error: Contact form not found.
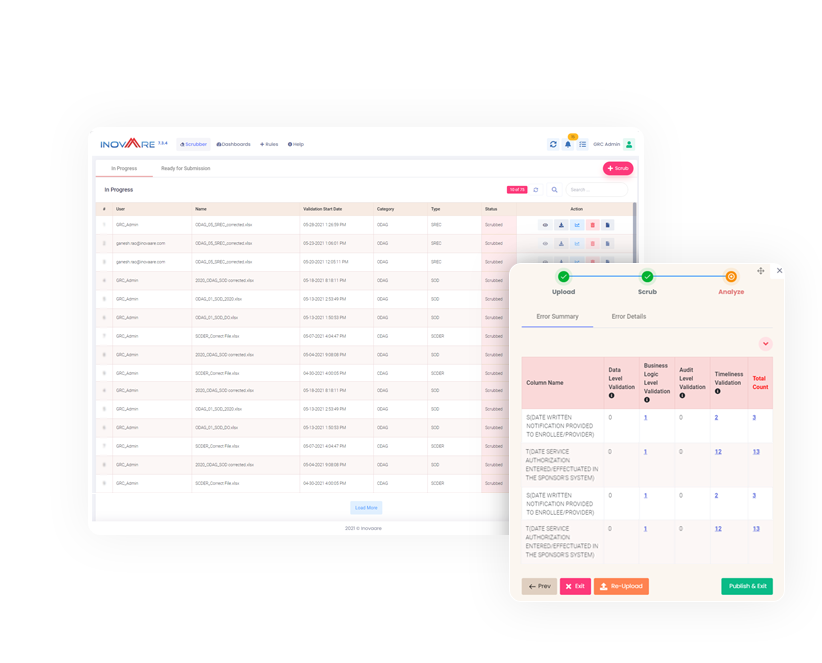
Traditionally, health plans commit resources for months while setting up all the data to comply with regulatory audits. Inovaare optimized the implementation process so that health plans can start using this powerful CMS universe validation and report generation tool within a week.
Inovaare’s Universe Scrubber scrubs Centers for Medicare and Medicaid (CMS) Program Audit universe reports and flags all crucial errors. This, alone, optimizes operational efficiency.
However, Universe Scrubber also analyzes universe tables for authorizations, claims, appeals and grievances CMS universes—such as Part C Organization Determinations, Appeals and Grievances (ODAG), Part D Coverage Determinations, Appeals and Grievances (CDAG) and Medicare-Medicaid Plan Service Authorization Requests, Appeals and Grievances (SARAG)—and other regulatory universes in real time. Payers can also monitor the health of their plans, on demand, by running Universe Scrubber monthly, weekly or even daily.
With all CMS universe tables embedded, Universe Scrubber provides access to real-time data so health plans can validate their CMS Program Audit universe tables in three simple steps:
Universe Scrubber empowers health plans to:
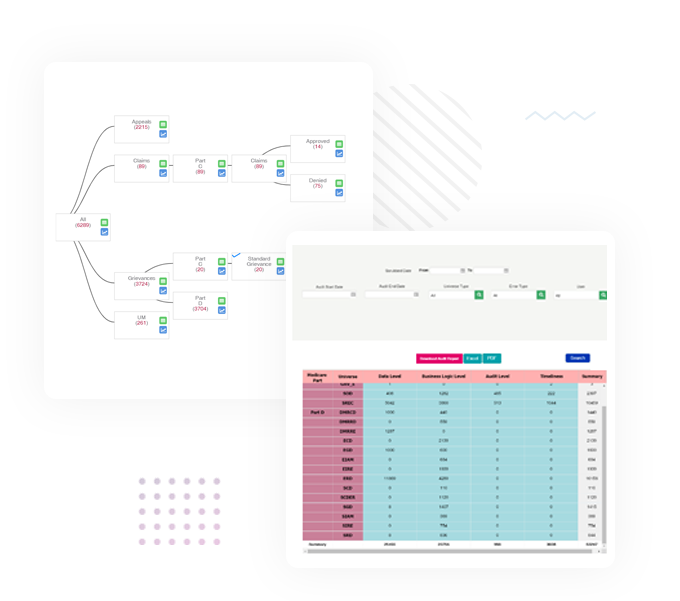
Health plans can reduce the risk of penalties and lower CMS Star Ratings by increasing report turnaround times. Universe Generator will do just that by enabling users to create properly formatted universes with the click of a button.
Universe Generator gathers data for requested date ranges to create clean universes for submission, even from multiple submitters providing the same universe table. It then compiles scrubbed universes into a single table for continuously compliant CMS report submission.
Universe Generator can be prebuilt with each report in the approved format for layout and data type and, when used regularly, this tool empowers payers to continuously monitor the health of their plans.
Additional benefits allow compliance teams to:

Work collaboratively with your delegated entities through our FDR Portal, which accesses and consolidates CMS Program Audit universes submitted by delegates. This efficiency ensures health plans can produce more accurate results with fewer resources to manage, monitor and audit FDRs.
FDR Universe Manager allows a health plan’s delegated entities to scrub and submit universes for review and potential remediation through a secure portal. This reduces the back-and-forth communication typically required for delegate universe submissions.
The automated workflow takes care of the manual processes to:

Most states require health plans to pay healthcare providers accurately and timely for their services. In parallel, payers must maintain a fast, fair and cost-effective system for processing and resolving provider claims. Health plans must also submit annual reports regarding the number, type and provider claim payment-dispute summaries. They are required to describe the resolutions including terms and timeliness and explain how they are addressing trends or patterns in disputes.
With Provider Dispute Resolution (PDR), health plans can:

The Quality Improvement Organization (QIO) Program, one of the largest federal programs dedicated to improving health quality for Medicare beneficiaries, is an integral part of the U.S. Department of Health and Human (HHS) Services’ National Quality Strategy for providing better care and outcomes at lower costs. CMS relies on QIOs to improve the quality of healthcare for all Medicare beneficiaries.
Inovaare’s QIO Appeals solution helps:
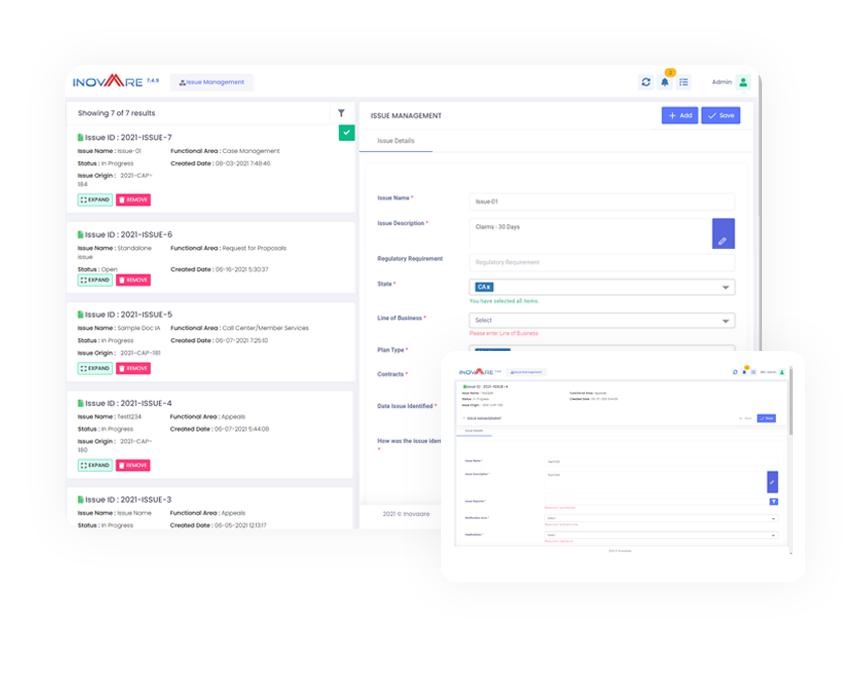
Architected by CMS regulatory compliance experts, Inovaare ensures health plans can effectively track and manage issues that have been identified as a risk or potential non-compliance. This includes automating corresponding follow-up actions and activities. Inovaare's Incident Management module empowers regulatory compliance management teams to drive continuous improvement activities across the entire enterprise. Now, payers can analyze trends, draw insights across multiple departments, implement and track corrective actions and then accurately measure real-time results.
Inovaare ensures health plans can:
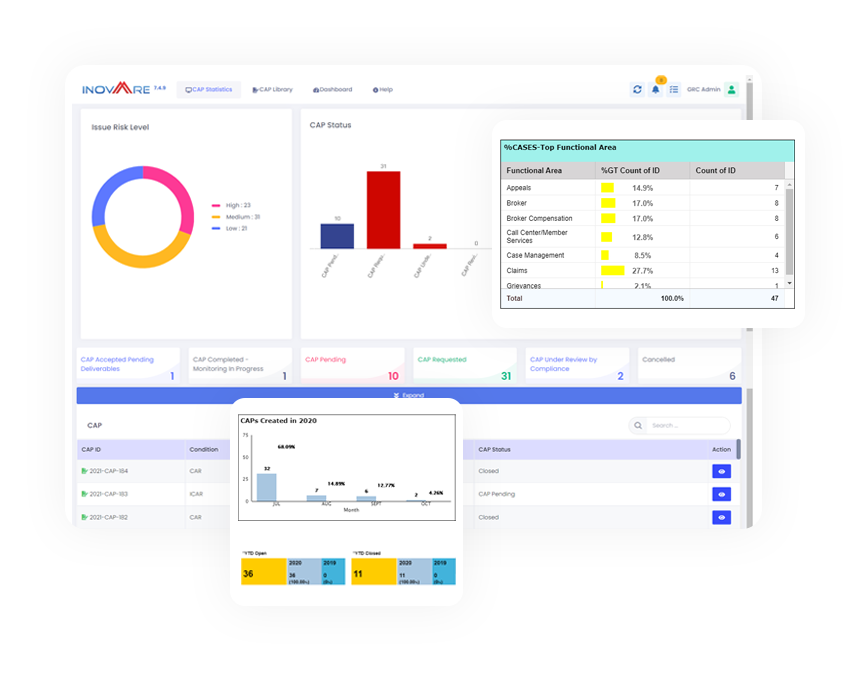
Inovaare’s Corrective Action Plan module automates CAP monitoring, assigns issues for resolution and records results of root-cause analysis. Now, health plans can:
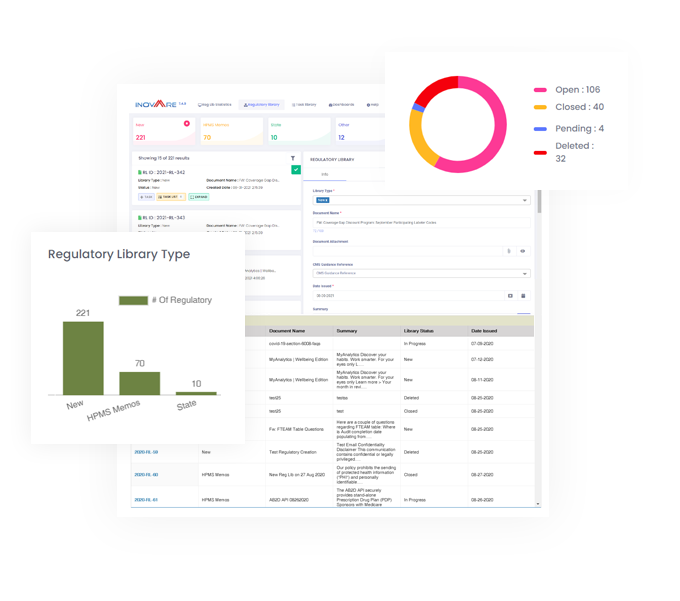
Inovaare’s cloud-based Regulatory Library module ensures an efficient process is in place to manage memos and ensure health-plan compliance is not consistently at risk. It equips health plans to streamline review processes and coordinate communication across all departments as well as update and monitor required due dates.
In addition to the ability to auto-load HPMS memos, efficiently monitor State Notices and improve department adherence to memorandums and quickly identify any corrective actions, health plans benefit from:
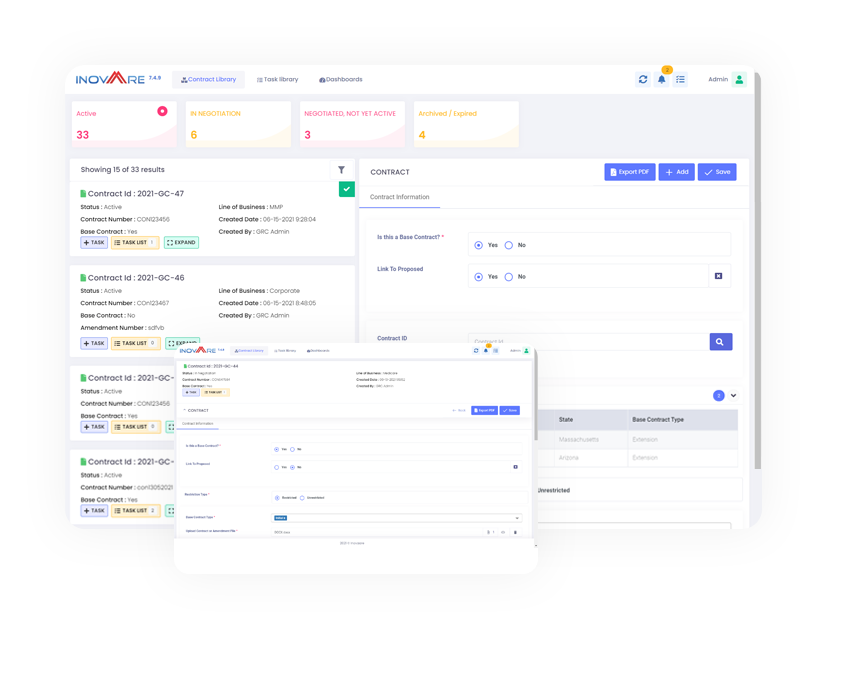
Enable proactive management of all contracts including those with vendors, service providers, customers and business partners. Facilitate collaboration using fully customizable workflow processes for review and approval.
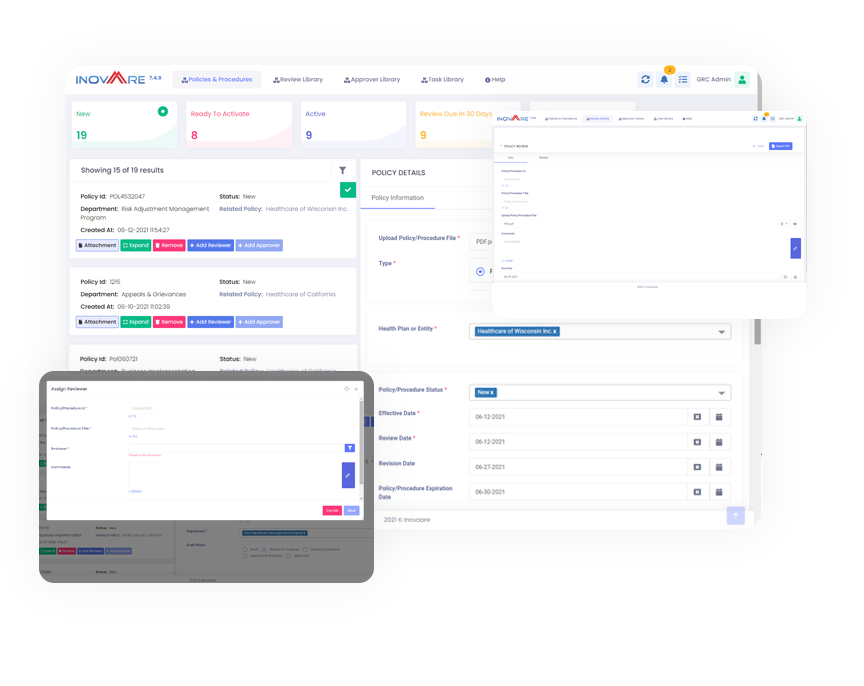
Policies and Procedures is a comprehensive cloud-based platform built for the healthcare industry that allows organizations to publish, assess and manage their policies and procedures. Health plans can create and/or review drafted policies, signoff and automate the full life-cycle management process of policies and procedures, including customizable workflows for review and approval.
Inovaare's cloud-based Contract and Policy Tracking module allows regulatory compliance management teams to:
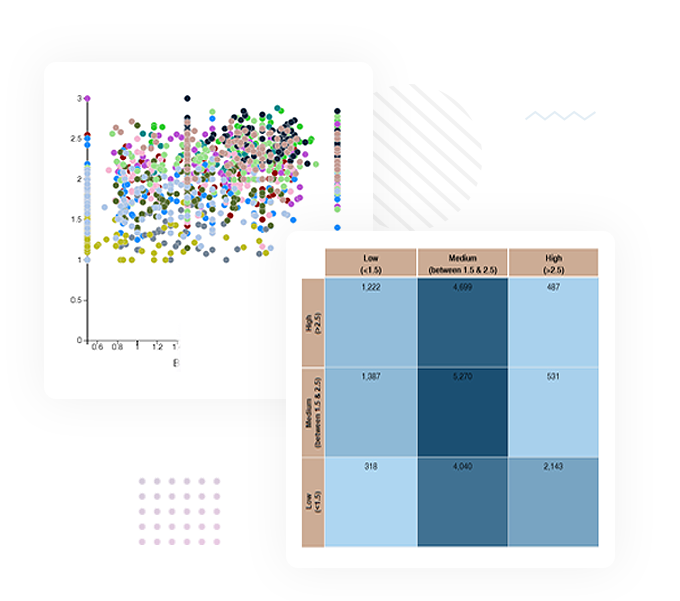
Inovaare’s Risk Management solution surveys and gathers evidence to determine risk. The module provides a single interface that users can access to create and edit attestations as well as change scoring parameters. Health plans can: complement existing risk-management policies and procedures with templates, metrics and workflows; minimize and manage corporate risks to lower the risk levels and reduce the organization’s direct costs; and maintain end-to-end audit trails.
Inovaare’s cloud-based Risk Management module empowers health plans to:
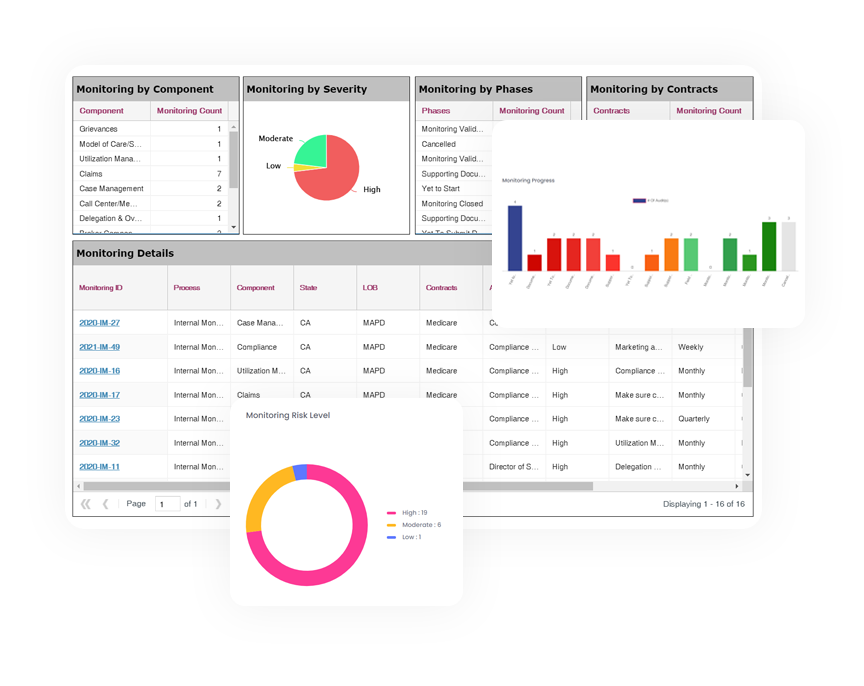
Demand for continuous risk management and control systems is on the rise, so organizations are adopting automation to support their audit teams. Inovaare’s Internal Audit module helps health plans manage end-to-end audit processes efficiently by delivering a systematic, risk-based audit system that streamlines workflows and provides real-time reporting. This allows health plans to attain a holistic view of the organization’s governance, risk and compliance status.
This cloud-based audit solution empowers health plans to:

Provider Disputes leverages Intelligent Automation to accelerate the resolution process for provider disputes and complaints. Provider Disputes is guided by a compliance rules engine which helps to ensure you stay compliant even when it is not top of mind. This robust solution offers all the necessary tools for Provider Dispute Leadership and PD Specialists to hyper-personalize each case until successful completion.

Health plans trust us to take their Customer Service, Appeals & Grievances and Provider Dispute Departments to a world-class level by incorporating our Industry-Leading Technology, implementing Best Practices, and adding our Expert Professionals to your team.
This BPaaS program includes the full suite of our solutions as well as industry experts who can fill all key operational Customer Service, Appeals and Grievances, and Provider Dispute roles. It also includes automated compliance solutions, which helps to elevate your A&G Department’s compliance adherence and operational efficiency.
With proactive regulatory updates, built-in rules and logic, and workforce management tools, it’s a holistic solution for healthcare organizations aiming to improve performance, achieve return on talent, and fast track the level of other high-performing health plans/organizations.
Best of all, our BPaaS quickly takes operational departments to the next level while also driving down the total cost of ownership.

Health plan leaders face complex challenges in member interactions across multiple channels. Ensuring seamless centralization and maintaining regulatory compliance in these interactions is crucial. These challenges include coordinating multiple departments for issue resolution and providing real-time access to customer histories, as well as the need to schedule future activities efficiently.
Inovaare offers a Member Services CRM solution tailored to the unique operational and compliance requirements of healthcare payers. Our platform streamlines the coordination process, enhances visibility across customer interactions, facilitates regulatory compliant reporting with ease, and supports health plans in delivering effective and compliant member services. The Member Services CRM—powered by real-time omnichannel and end-to-end workflow automation—delivers improved member experiences through more efficient processes.
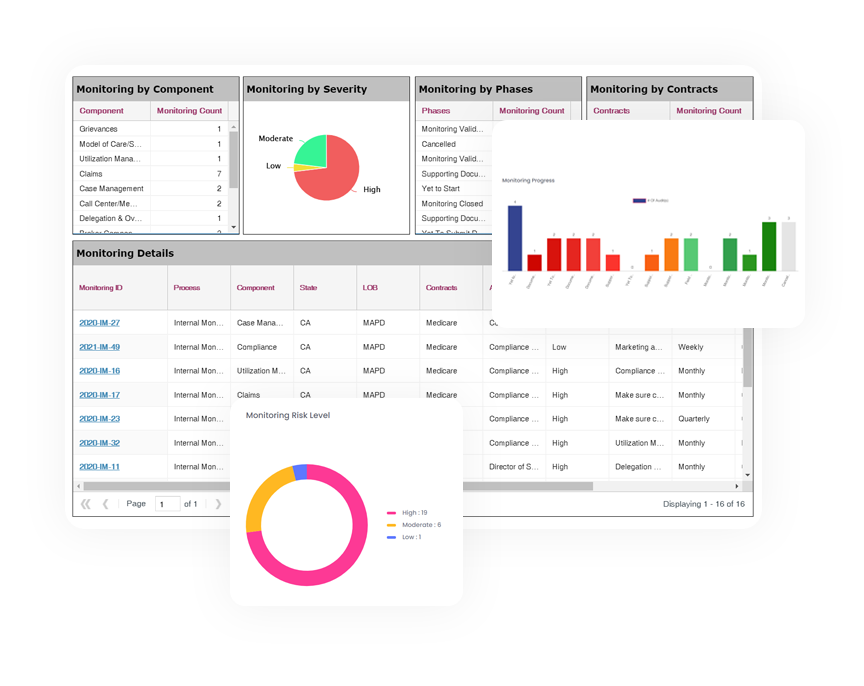
Sustaining compliance is a challenge, since CMS and state regulatory requirements change frequently. However, by implementing internal checks and reviews, health plans can gain better visibility of their quality control and compliance processes.
Continuous monitoring of your compliance program not only helps improve operational health, but it demonstrates to the CMS that your health plan takes compliance seriously. Inovaare’s Internal Monitoring solution assists health plan to:

External auditors are essential to ensure health plans meet their governance, risk management and compliance (GRC) requirements. Inovaare’s External Audit solution enhances the exchange process through its compliance-driven platform.
Embedded with all applicable federal and state regulations — including Medicare Part C, Medicare Part D and Medicaid — this cloud-based module helps heath plans to:
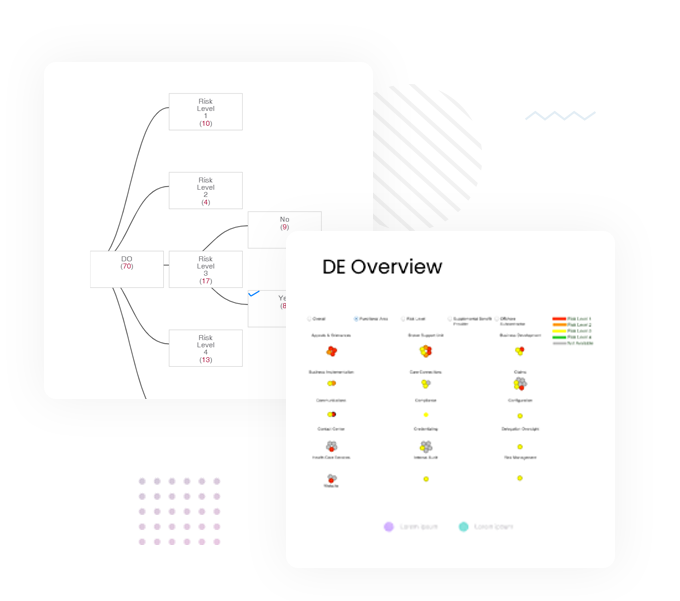
Inovaare’s Delegation Oversight module enables health plans to manage first-tier, downstream and related (FDR) delegated entity compliance. Now, Delegation Oversight departments can perform systematic reviews of FDR operations—to ensure they are in line with business requirements—while empowering plan sponsors and MCOs to manage and track all audits and monitoring of delegated entities. The module also provides a secure portal for communication where delegated entities can scrub their universe files before submitting them to the health plan.

Experience the difference. Inovaare’s CRMؙ—Member Services is the only solution that shares the same platform as Appeals & Grievances and CRM—Provider Services. This singular platform delivers better member experiences powered by end-to-end workflow automation. Inovaare’s CRM—Member Services was architected by leaders who oversaw Member Services departments and, as a result, we understand your requirements for Medicare, Medicaid and Commercial plans. Our industry-leading solution helps health plan to:
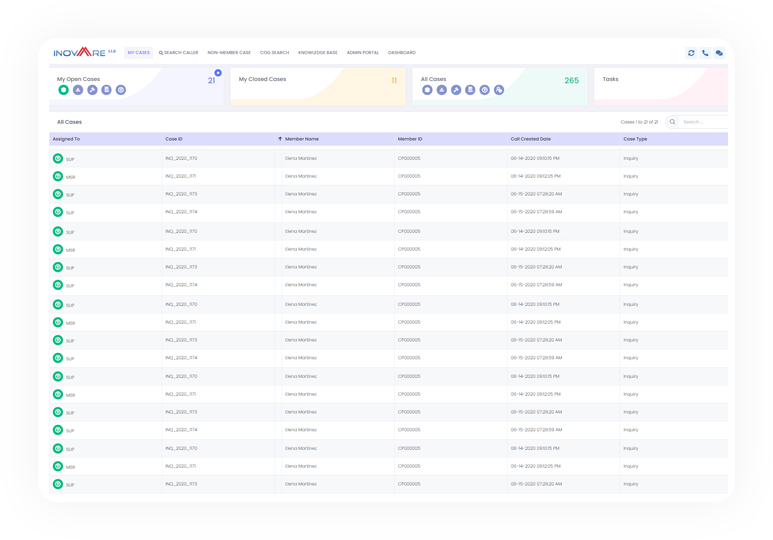
Experience the difference. Inovaare’s CRM—Provider Services is the only solution that shares the same platform as CRM—Appeals & Grievances and CRM—Member Services. This singular platform delivers better provider experiences powered by end-to-end workflow automation. Inovaare’s CRM—Provider Services was architected by leaders who oversaw Provider Services department and, as a result, we understand your requirements for Medicare, Medicaid and Commercial plans. Our industry-leading solution helps health plans to:

Streamline your operations with Inovaare's Workflow Automation, designed for efficient process management and enhanced productivity.

Ensure data integrity with Inovaare's Data Platform, utilizing sophisticated rule-based controls for impeccable data quality.

The Analytics & Reporting component is engineered to empower healthcare payers with deep insights and comprehensive reporting capabilities. The data platform sees data as a strategic asset and intelligently transforms complex data into actionable intelligence, helping organizations drive operational excellence, be on-point with compliance, and enhance strategic decision making.
Seamless Data Management, Compliance, Operations, and Member Service
Inovaare offers an AI-powered platform that simplifies app development by eliminating infrastructure complexities. It includes tools for design, development, testing, and deployment, along with necessary infrastructure like servers and networking. Inovaare’s modern platform also features a marketplace of pre-built compliance solutions for health plans, enabling quick deployment of new applications. Inovaare brings you a cloud infrastructure that is scalable, cost-effective, and secure.



Automate and optimize processes to enhance productivity.
Create and store compliance and business rules to ensure data quality.
Turn complex data into actionable intelligence, enabling efficient and swift data-driven decisions.
Implement ready-to-use solutions with configurable workflows.
Pause and resume your apps as needed.
Secure, HIPAA-compliant, and
HITRUST CSF®-Certified cloud.
Experience out of box BI platform connected with data in real time.
Create custom apps using the low code no code platform.
Seamlessly integrate with your existing systems and data sources.

Retrieve information faster with AI-powered search capabilities. Usher uses natural language processing to understand queries and provide precise results.
Go beyond basic search with Usher. Analyze search patterns and results to refine your information strategy and improve future searches.
Engage with our AI chatbot for instant assistance. Usher answers questions, guides users through complex processes, and improves user experience.
Harness the power of AI to interpret and analyze text data. Usher provides sentiment analysis, keyword extraction, and thematic categorization.
Scale and adapt effortlessly with dynamic, flexible architecture.
Minimize large initial investments in hardware and ongoing maintenance.
Agile deployment for rapid adaptation to market and regulatory changes.
Advanced security and compliance features for privacy of sensitive data.
Integrated data analytics, BI platform, and AI capabilities.
Seamless connectivity with digital healthcare networks and technologies.





Leverage Inovaare’s Solution Architecture Consulting service to get custom, scalable healthcare solutions. Our experts design robust, future-proof systems that comply with current regulations and adapt to new technologies.
Inovaare’s Solution Configuration Support ensures your healthcare platform is tailored to your workflow, fine-tuning your processes, roles, and data needs for a seamless organizational integration.
Inovaare provides comprehensive Healthcare Compliance Support, keeping up with regulations and integrating them into your platform, ensuring your operations stay compliant and prepared for regulatory changes.


Choose from a range of templates or start from scratch.
Add components, define workflows, and integrate data sources.



Launch your app and see your innovation in action.
Automate routine tasks to minimize manual processes allowing staff to focus on more valuable work.
Low-code/no-code platform reduces the need for technical resources and speeds up go-to-market.
Automated compliance features ensure audit readiness, saving on audit preparation costs and time.
AI-powered analytics lead to more effective strategies resulting in higher member retention.
Empower your operational teams to scale without proportional increases in costs or resources.
Strong data protection measures prevent breaches, protecting against loss and reputational damage.
Seamless data exchange and interoperability with external systems like HL7, EDI, and PHIR.
The ability to rapidly develop and deploy new applications pushes innovation, leading to competitive advantages.
Securing your data is most important to you, and Inovaare does it as per industry best practices.

Secure hosting and built-in safeguards protect your app and user data at all times.

Advanced DDoS protection ensures uninterrupted service and data security.

Inovaare platform ensures data confidentiality and protection with advanced encryption.

Advanced monitoring services ensure protection of your digital assets.
Inovaare designs HIPAA-compliant health-plan software—built on an end-to-end regulatory compliance, operations and audit-management data platform—to streamline CMS and state regulatory reporting requirements and quality improvement processes. This innovative and intuitive cloud-based platform automates data collection from complex health plan processes across disparate departments to create a centralized, integrated information management system.
Data security is essential in healthcare and Inovaare has its clients covered. Its qualified and certified IT security experts manage data security to keep up-to-date regarding the latest global threats and risks. Inovaare performs internal and external assessments to ensure that all necessary elements are checked—from an information security perspective—as well as to make sure data is secured at all times.
Inovaare’s information security objectives are amalgamated into cross-cloud platforms where its software-as-a-system (SaaS) solutions reside. This way, Inovaare can ensure it delivers consistently reliable solutions with high uptime, uninterrupted availability and iron-clad data security.


The Inovaare Platform stands out for its ability to deliver customized, efficient solutions specifically designed for the healthcare industry. It combines cutting-edge technology with user-friendly features to streamline compliance, operational efficiency, and data management. With Inovaare, you can leverage advanced analytics, AI-powered tools, and robust security measures, ensuring they stay ahead in a rapidly evolving regulatory landscape while optimizing patient care and business outcomes.
Inovaare is proudly powered by WordPress
